Warning: this will hurt your brain.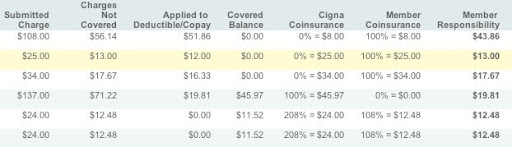
I’m baffled. I know that “Submitted Charge” is the amount the provider submitted. “Charges Not Covered” is the difference between the submitted charge and the negotiated (or contracted) price that Cigna has agreed to pay for the mystery service. We have a $100 copay, so the negotiated price is applied to the deductible until we hit $100, and then it shifts over to “Covered Balance.” So on the first line, 108–56.14=51.86. Fine. But then how is Cigna getting to $8 under “Cigna Coinsurance” and $8 under “Member Coinsurance”? And what are they 0% and 100% of? Well, $8 is 100% of the submitted charge of $108 less the copay of $100, but that makes no sense because the coinsurance is supposed to be calculated based on the negotiated price, not the submitted charge. And $8 isn’t 0% of anything, even with rounding. This utter nonsense continues on the next two lines, where the percentages and the dollar values are completely disconnected.
So how was the final column, “Member Responsibility,” calculated? In the first line, it’s the negotiated price minus either the Cigna coinsurance or the member coinsurance. But on the second and third lines, it’s the charges not covered. On the fourth line, it’s the amount that was applied to our deductible, which is also the negotiated price minus the Cigna coinsurance. So it’s possible that there were only two different calculations used in the first four lines to figure out the Member Responsibility. And one of those calculations might be right.
The fourth line looks like it could be right. We pay $19.81 towards our copay, reaching $100 total, and then the remainder of the negotiated price is paid by Cigna. If the member responsibility is supposed to duplicate the copay amount, then that line is ok.
But then we reach the magical fifth line. Cigna’s coinsurance suddenly jumps to 208%, while the member coinsurance jumps to 108%, for a total coinsurance of 316%. That’s a lot. Strictly as a percentage, 108% is 100 points less than 208%, so it’s the absolute value of X (|X|%) in the formula 208% + X% = 100%, since the two coinsurance percentages should total 100%. And I cannot imagine a reason that a set of calculations like this should ever be using absolute value to convert negative amounts or percentages into positive ones.
Why is Cigna’s coinsurance the exact amount of the submitted charge, and why is the member coinsurance the exact amount of the charges not covered? The total of the two coinsurance payments should be the negotiated price, which is neither of those numbers (and in fact is smaller than either of those numbers).
Perhaps the details are the problem, and I should just look at the totals. The EOB ends up with a total copay of $100 (which is correct), a total member coinsurance of $91.96 (which is not correct), and a total member responsibility of $119.30 (which is neither correct nor connected to the first two numbers). On the summary of claims page, which links to individual EOBs like this one, the total member responsibility is listed as $8.04. That happens to be the difference between the total copay and the total member coinsurance, but there’s no reason why that calculation should ever be done. Nor any reason why the total member responsibility should be different on the summary page and on the EOB.
How an EOB should be calculated
(A) Submitted Charge: A
(B) Negotiated Price (not shown): B
(C) Charges Not Covered: C=A–B
(D) Applied to Deductible/Copay: D=B until deductible/copay is reached, then D=0
(E) Covered Balance: E=B–D
(F) Cigna Coinsurance after out-of-pocket limit is reached: F=100% of E
(G) Member Coinsurance after out-of-pocket limit is reached: G=0% of E
(H) Member Responsibility: H=D+G
How Cigna works
(F) Cigna Coinsurance after out-of-pocket limit is reached: F=A–copay, or F=A, or F=E
(G) Member Coinsurance after out-of-pocket limit is reached: G=F, or G=A, or G=0% of E, or G=C
(H) Member Responsibility: H=D–F, or H=D+G, or H=C
My brain hurts. How’s yours?
Wednesday, June 18, 2008
Cigna math: inexcusable
Subscribe to:
Post Comments (Atom)

4 comments:
When I called and asked Cigna to take a look at this EOB and explain it to me, the rep said that it wasn’t really clear.
This is a self-insured plan, so the employer pays all health care expenses that are reimbursed by the plan. Cigna is not the insurer; they simply process claims and are paid a small percentage of the total (probably around 2% to 6% of the total). For the employer, this is rather like hiring a payroll company to process the payroll. But if people’s paystubs arrived looking like this, the employer would fire the payroll company.
Michael -- As a CIGNA representative, I was sad to see the confusion caused by our EOB, but was pleased to see our service team was able to address the issue to your satisfaction. Clearly we need to improve our EOB, and we are: our medical EOB is being completely redesigned with much better layout, clearer labeling and easy to understand descriptions.
Simply put, we're committed to improving your experience with CIGNA, and look forward to serving you better the next time around. Meantime please accept this apology and explanation; we expect to do better in the future.
Joe -- Thank you for posting, but Cigna absolutely did NOT address the issue to our satisfaction. The Cigna service team did not address the issue at all. The EOB is incomprehensible and clearly wrong in many ways, and the only response from Cigna was a complete understatement that it wasn’t really clear.
I’m glad to hear that Cigna is planning to improve the EOB statements. The layout needs work, and the lack of content is frustrating. But without getting the math right, the rest of it is cosmetic fixes. And until Cigna stops hiding CPT codes from members, and stops lying about the reasons, the EOB situation will not be sufficiently improved.
Curiously, two weeks after promising to send this nonsensical EOB back to their own claims department for reprocessing, Cigna mailed us another copy of it with nothing fixed. If they didn’t change anything, why mail us another copy?
Post a Comment